All posts
Inside America’s sleep struggle: How restlessness is taking a toll on mental health

Circle Medical Staff
Aug 13, 2025
5 minutes

Across the U.S., people aren’t just feeling tired, they’re feeling unwell. Sleep isn’t something they’re missing occasionally, it’s something they’re struggling with night after night and it’s taking a toll on both energy levels and emotional health.
According to our latest survey*, 47% of Americans say they’ve experienced poor or very poor sleep in the past two weeks, with only 31% reporting good sleep and 38% describing their rest as just “fair.”
For many, this isn’t a short-term slump. 59% say they struggle to fall asleep at least once or twice a week, and one in five face that struggle every single night.
This nationwide sleep deficit is more than a matter of fatigue, it’s driving up anxiety, draining motivation, and making everyday life harder - and people know it.
Search trends reveal a nation looking for answers
Recent Google search trends reflect the rising anxiety levels around sleep in the States. In July 2025 alone there was:
- Over 1.2 million searches for “sleep apnea”
- Over 3,000 searches recorded for “sleep apnea and depression” - an increase of 179% compared to the previous month
- A rise in other breakout terms including “CBT for insomnia,” “how to fall asleep faster,” and “best sleep hygiene”
This real-time data mirrors our survey findings: Americans are actively looking for solutions, not just for how to fall asleep but for how to break the cycle of bad sleep and worsening mental health.
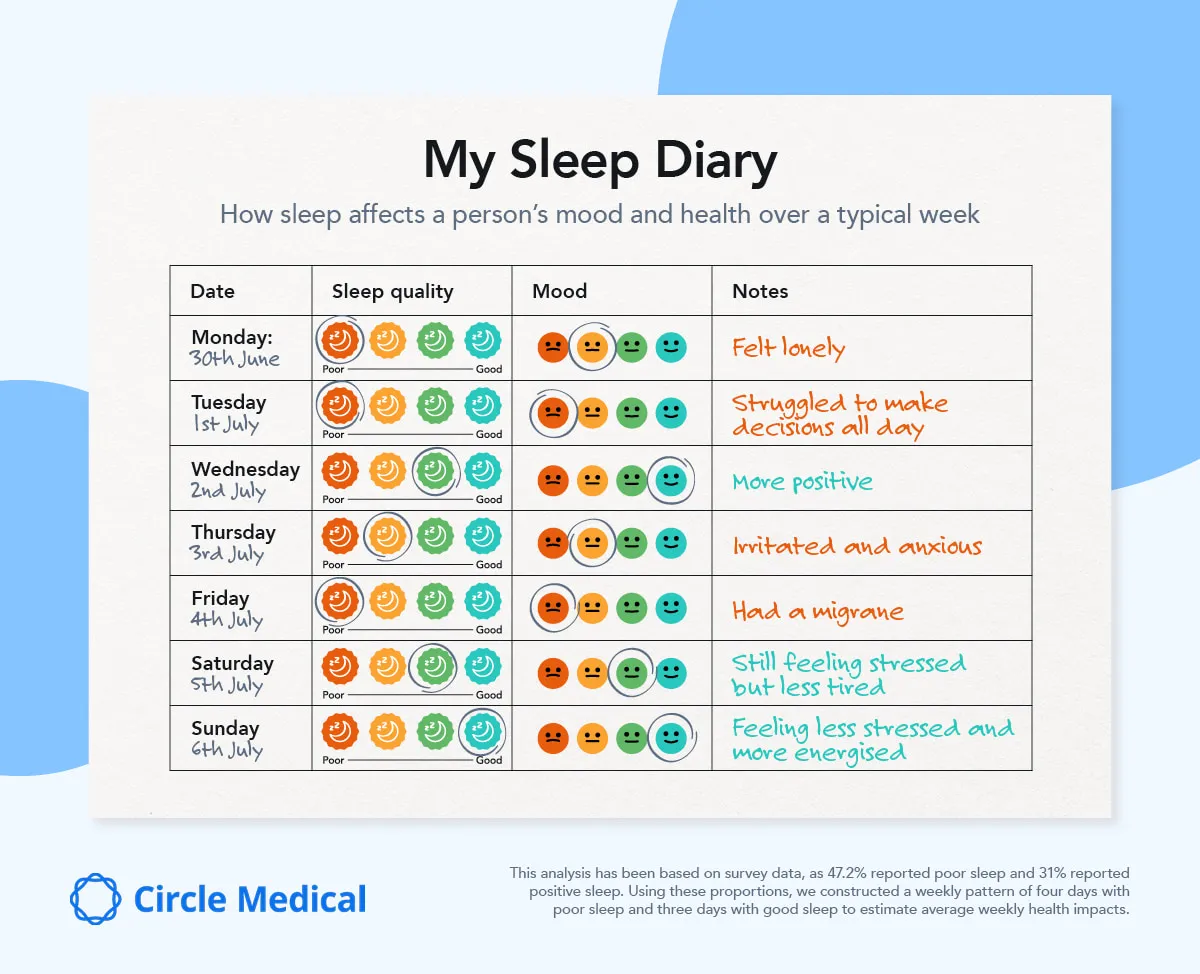
The real-world impact of poor sleep
What exactly are people feeling when they sleep badly?
Our data reveals that for 83% of people, their mood is negatively affected by poor sleep, and 82% say it also impacts their overall mental well-being.
A strong connection between sleep quality, stress, and cognitive difficulties was revealed, highlighting a vicious cycle where stress disrupts sleep, and poor sleep in turn amplifies stress and impairs focus - trapping many in a challenging loop.
- 78% of respondents agree that poor sleep makes it harder to concentrate
- 75% report that their stress levels impact their sleep quality
- 71% say they struggle to concentrate more when they have poor sleep
Specifically, the 10 most common symptoms reported after a poor night’s sleep include:
- Low energy (56%)
- Tiredness throughout the day (54%)
- Fatigue (51%)
- Lack of motivation (38%)
- Anxiety (32%)
- Low mood (28%)
- Struggle to concentrate or pay attention (27%)
- Headaches or migraines (26%)
- Trouble remembering or thinking (24%)
- Mood swings (23%)
Sleep is also affecting how people engage with others: 43% said poor sleep makes them want to cancel all their plans, highlighting just how much rest influences both physical and emotional bandwidth.
And while the “Sunday Scaries” are a well-known cultural phenomenon, our data suggests that for many, that sense of dread and tension is no longer confined to just Sunday evenings. For nearly one in five people, stress and restlessness are now nightly battles.
People are trying to sleep better but many are getting it wrong
Despite the severity of the impact, people aren’t ignoring the problem. 83% of respondents say they’re actively trying to manage their symptoms, and 70% are regularly seeking new ways to improve sleep quality. But their methods vary and many common habits aren’t supported by sleep science.
Here’s what our respondents are trying and how those strategies are stacking up:
| Strategy used to improve sleep | Respondents | Clinical impact |
|---|---|---|
| Going to sleep earlier | 41% | ✅ Effective |
| Taking sleeping pills | 28% | ⚠️ Dependent on severity |
| Consuming energy drinks and caffeine late in the day | 27% | ❌ Counterproductive and a short-term fix |
| Turning off screens before bed | 26% | ✅ Effective |
| Eating earlier in the evening | 20% | ✅ Effective |
| Exercising too close to bedtime | 17% | ⚠️ May delay sleep |
| Drinking alcohol to unwind | 15% | ❌ Disrupts sleep |
| Hitting snooze repeatedly | 14% | ❌ Fragments sleep |
While some tactics, like dimming lights or setting earlier bedtimes, align with expert guidance, others may be doing more harm than good.
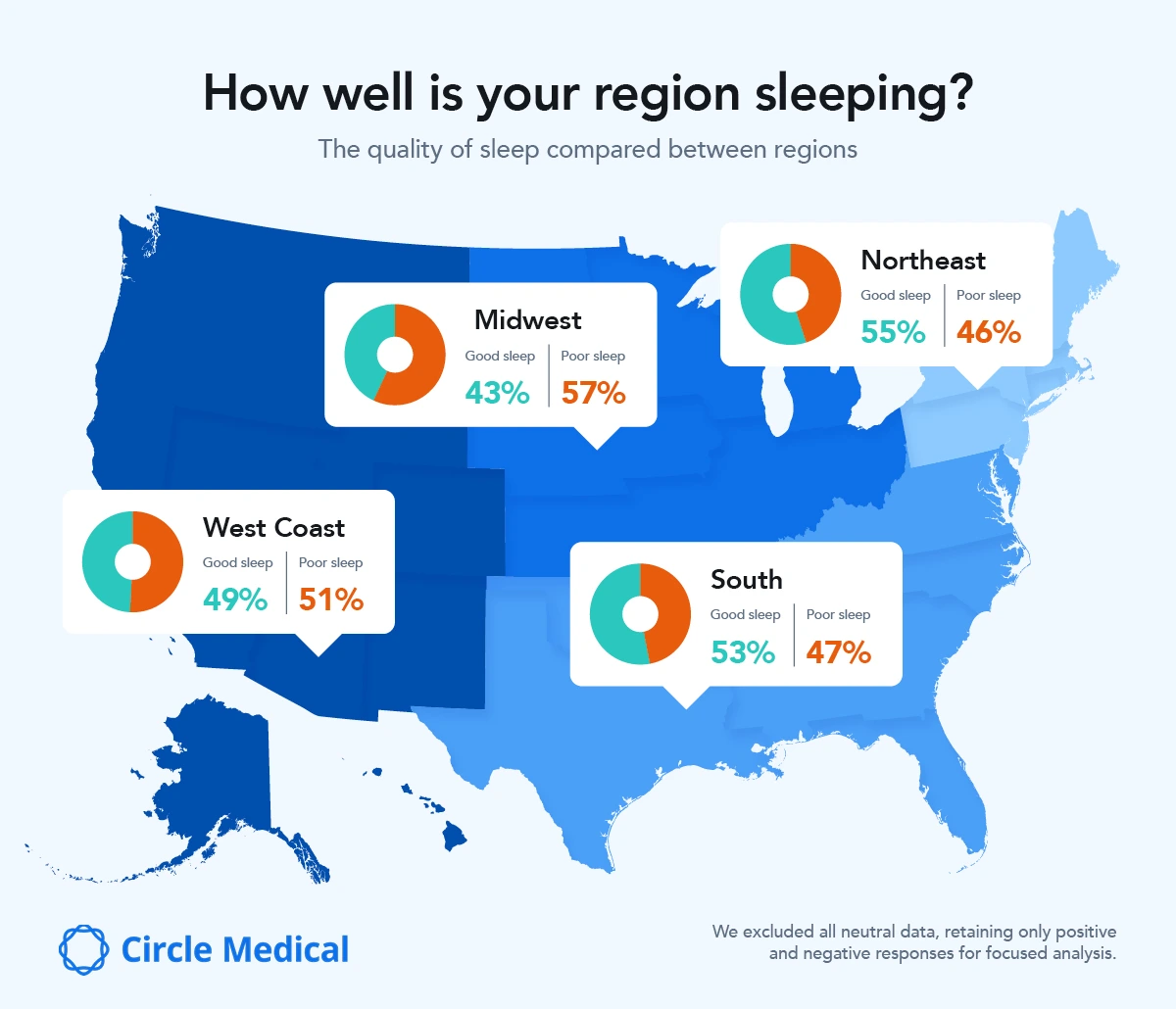
Where in the country are people sleeping the best and worst?
While poor sleep is a national concern, a closer look at regional trends revealed significant differences in both sleep quality and how people are coping with it.
The Midwest is losing the most sleep
Sleep struggles are most severe in the Midwest, where 38% of people rate their sleep as poor - the highest percentage in the country, with only 28% reporting good quality sleep.
This imbalance may contribute to higher stress and concentration issues across the region, continuing the cycle of poor rest and mental fatigue, especially as only 49% of respondents lean towards safe and effective methods.
The West is falling behind
The West is close behind the Midwest in poor sleep, with 33% of respondents rating their sleep quality as poor. What’s more, the West also relies most heavily on bad habits to cope, with 28% admitting to poor sleep hygiene routines and 22% depending on potentially harmful methods like alcohol or medication. Only 49% take a healthier approach, at a similar rate to the Midwest.
The South sits somewhere in the middle
In the South, sleep habits fall somewhere between the extremes. 29% report poor sleep, while 32% rate their sleep as good. Solutions are similarly mixed, just 51% rely on positive sleep strategies, while 24% use coping methods considered dependent or unhealthy, such as alcohol or late-night stimulants.
The Northeast is sleeping the best and solving it better too
On the other hand, people in the Northeast report the best sleep, with only 28% saying their sleep is poor and 32% enjoying good sleep regularly. Perhaps more importantly, Northeasterners are also addressing their sleep issues more effectively, with over half (54%) using healthy solutions like exercise, reducing screen time, or consistent sleep routines. Just 24% are turning to unhelpful habits or bad routines.
Gender gaps in sleep and mental health effects
Sleep struggles aren’t affecting everyone equally either. The survey data revealed clear gender differences, with men reporting better sleep (35%) than women (27%).
Women are more likely to experience poor sleep, with 34% reporting issues in the past two weeks - compared to 28% of men. The difference is just as pronounced when it comes to mental health too, with more women experiencing anxiety, lack of motivation, and mood swings than men.
| Symptom | Women (%) | Men (%) |
|---|---|---|
| Anxiety | 35.4 | 28.4 |
| Low mood | 31.7 | 24.2 |
| Mood swings | 25.9 | 20.7 |
| Feeling more stressed | 33.9 | 29.8 |
| Lack of motivation | 43.7 | 32.5 |
Understanding these differences is key to addressing the sleep crisis. Sleep solutions must reflect that women may need more targeted support to break the cycle of poor sleep and its negative impact on mental health.
How to actually improve sleep and mental health alongside it
A better night’s sleep doesn’t just mean feeling rested. It can also mean lower anxiety, improved mood, and higher daily motivation. Achieving this takes more than one-off tricks, as it requires a consistent, evidence-backed routine.
Clinician, Dr. Nicole Tsang at Circle Medical, said: “If your sleep feels unrefreshing no matter what you do, talk to a provider. You may need a clinical assessment or a sleep study, especially if you’re also experiencing mood changes, memory issues, or low motivation.”
Dr. Nicole Tsang shares what works:
1. Create a wind-down routine
Start relaxing 60–90 minutes before you go to sleep. This can include reading, dim lighting, or gentle movement; anything that signals to the brain that rest is coming.
2. Avoid caffeine after 2 p.m.
Caffeine’s long half-life means it can still be in your system when you’re trying to fall asleep and reduce sleep quality even if you do manage to drift off.
3. Time exercise earlier
Exercise improves sleep, but doing it within two hours of bedtime can delay melatonin release. Aim for morning or early afternoon workouts instead.
4. Ditch alcohol as a sleep aid
Alcohol may help you fall asleep faster, but it fragments your sleep cycles and reduces the amount of REM — the most restorative sleep stage.
5. Address racing thoughts
Anxious thinking is one of the biggest barriers to sleep. Journaling, CBT-I techniques, and even simple breathing exercises can help to reduce nighttime mental overload.
6. Rule out sleep apnea
Many people who say they “slept 8 hours but still feel exhausted” may be dealing with undiagnosed sleep apnea, which is a condition where breathing is repeatedly interrupted during the night. It’s a known risk factor for both depression and anxiety, yet often goes untreated.
Sleep is more than rest, it’s mental resilience
This study makes one thing clear: Poor sleep is more than a nightly nuisance, it’s a daily mental health issue for many. Across regions, routines, and responses, the data reveals a nation stuck in a cycle: Stress and anxiety disrupt sleep, and bad sleep makes stress harder to combat.
Dr. Nicole Tsang added: “If we want to improve our mental well-being, we need to start with our sleep. That means not just reacting to poor rest but preventing it: setting healthier boundaries with screens, building routines, and making sleep a non-negotiable part of wellness, rather than an afterthought.
“When you know your sleep, you begin to know your mind.“
Methodology:
- The survey was conducted by Circle Medical in June 2025 with a nationally and gender-representative sample of 1,000 U.S. adults.
Google search data was collected in July 2025.
Circle Medical Providers must meet all of the following standards:
-
Exceptionally qualified in their field
-
Board-certified
-
Deeply empathetic for patients
-
Follows evidence-based care guidelines
-
Embracing of diverse patient backgrounds
-
Impeccable record of previous care
400+ Primary Care Providers.
100% Confidence.
No matter which Provider you choose, you will be seen by a clinician who cares deeply about your health and wants to help you live your happiest, healthiest life.
Circle Medical Providers are held to an exceptionally high standard of compassionate, evidence-based care.
Book Appointment